Retinal Vascular Disorders
Back to Basics – Retinal Disorders
Retinal Vascular Disorders
What are Retinal Vascular Disorders?
Retinal vascular disorders refers to a range of eye diseases that affect the blood vessels in the eye. These conditions are linked back to pre-existing vascular diseases such as hypertension (high blood pressue) and arthrosclerosis (thickening of the artery walls). The most common retinal vascular disorders which we will be discussing in this article are:
- Hypertensive Retinopathy
- Central Retinal Vein Occlusion (CRVO)
- Central Retinal Artery Occlusion (CRAO)
- Ischaemic Optic Neuropathy (Optic Nerve Atrophy)
- Diabetic Retinopathy (Read our article on Diabetic Retinopathy here: https://sosdoctors.com.au/back-to-basics-diabetes-and-diabetic-retinopathy/ )
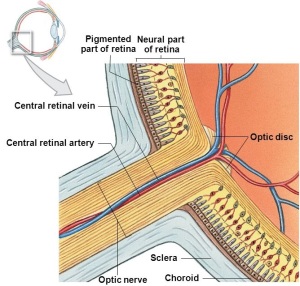
Retinal Blood Supply
The outer Retinal pigment epithelium (RPE) and photoreceptors are supplied by the Choroid. The inner neural retina is supplied by the central retinal artery. The central retinal artery then divides into two equal superior and inferior branches nasally and temporally, which supply all of the inner layers of the neural retina, with corresponding venous drainage.
a. Hypertensive Retinopathy
Hypertension causes the blood vessels in the eye to narrow, leak and harden over time. In some cases this can cause the optic nerve to swell and affect vision. You have a higher risk of damage to the blood vessels in your eye if you have diabetes, high cholesterol or you are a smoker. Most people with hypertensive retinopathy do not have symptoms until the later stages of the disease. Symptoms may include headaches, double vision (diplopia), dim vision or vision loss.
Risk Factors
Risk factors for hypertension include a high salt diet, obesity, smoking, alcohol, family history, stress & ethnicity. The major risk factor for hypertensive retinopathy is the length of time blood pressure has been elevated.
Treatment of Hypertensive Retinopathy
The main objective of treatment of hypertensive retinopathy is to address the hypertension – through medication and lifestyle changes.
b. Central Retinal Vein Occlusion (CRVO)
A central retinal vein occlusion, or CRVO is a blockage of the main vein in the retina. Blockage of the smaller veins in the retina are referred to as Branch retinal vein occlusion (BRVO). The blockage causes the walls of the vein to leak blood into the retina. When this fluid collects in the macula vision becomes blurry. There are two different types of CRVO: Non-ischemic CRVO and Ischemic CRVO. Ischemic CRVO is more serious of the two types and can lead to loss of vision in the affected eye. The main cause of CRVO is the formation of a blood clot. This usually occurs when a retinal artery crosses over a vein, slightly constricting it, resulting in blood flow being slowed down. When blood flow slows, the blood tends to thicken and forms a clot.
Risk Factors of CVRVO
Risk factors for CRVO are the same that we have listed for hypertensive retinopathy above with the addition of elevated cholesterol and poorly controlled diabetes.
Symptoms of CRVO
Most people with CRVO notice a gradual, painless loss of vision. However if the blocked vein is in the peripheral retina – and therefor away from the macula – there may be little or no vision loss noticed.
Treatment of CRVO
Treatment of CRVO will depend on the nature, location and size of the blockage. As is the case for many retinal conditions, laser and or Anti-VEGF injections are both possible treatment options.
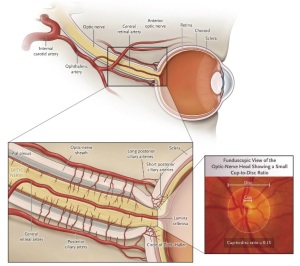
c. Central Retinal Artery Occlusion (CRAO)
A central retinal artery occlusion, or CRAO is considered an ocular emergency and is caused by a blockage of the central retinal artery. Blood clots may travel from other parts of the body and cause a blockage to the central retinal artery. The most common source of such clots are the heart and carotid artery.
Risk Factors of CRAO
The risk factors for CRAO are the same atherosclerotic risk factors for stroke and heart disease: Most blockages occur in people who have conditions such as Diabetes, Carotid artery disease, atrial fibrillation (a problem with the heart’s rhythm), hyperlipidemia (high levels of fat in the blood), high blood pressure, temporal arteritis or have a history of intravenous drug abuse. Individuals with CRAO may be at risk of a cerebral vascular accident (stroke).
Symptoms of CRAO
The sudden, painless complete loss of vision to one eye.
Treatment of CRAO
The American Academy of Ophthalmology advises that “Acute treatment to limit visual acuity loss is usually effective within 90 minutes of onset”. Given time to act on this condition is so limited, we emphasise the urgent nature of seeking help. Breathing into a paper bag increases carbon dioxide content which causes the vessels to dilate. This is recommended as an immediate first response to the sudden loss of vision & should be continued until you are seen by an ophthalmologist. Those suffering from a central retinal artery occlusion have an risk of stroke and heart disease. For this reason, the management of CRAO is not only to attempt to restore vision but to manage these associated risk factors. To date, there are a number of therapies used to attempt to restore vision after a CRAO, however the success rate of these therapies has proven to be very low with a poor visual prognosis following a blockage of the central retinal artery. Vision loss
d. Ischemic Optic Neuropathy (ION)
The AAO defines Ischemic Optic Neuropathy as a “sudden loss of central vision, side vision or both due to a decreased amount of blood supply to the eye’s optic nerve”. The optic nerve is made up of a million tiny, delicate nerve fibres that are like wires. There are many blood vessels that nourish the optic nerve with blood rich in oxygen and nutrition. If the optic nerve is not healthy and nourished, vision is not possible. Click image below to enlarge
Types of ION
There are two types of ischemic optic neuropathy which is dependent on the part of the optic nerve involved:
- Anterior Ischemic Optic Neuropathy (AION) which occurs when blood flow in interrupted to the front (anterior) part of the optic nerve.
- Posterior Ischemic Optic Neuropathy (PION) which is much less common and is a result of interruption to blood flow to the back (posterior) part of the optic nerve – the location of which is behind the eyeball.
Most cases of ION fall under the category of AION. AION is further subdivided into two different types:
- Arteritic AION: This dangerous form of AION is caused by inflammation of the arteries supplying blood to the optic nerve. Arteritic AION, is three times more common in women than men and affects those over the age of 55.
- Non-Arteritic AION: Nonarteritic anterior ischemic optic neuropathy (NAION) is the most common form of AION. NAION can affect someone at any age, with about 10 percent of those affected younger than 45. Men and women are equally at risk.
Fluorescein angiography may help confirm the blockage of blood flow in an arteritic AION.
Causes of ION
As with each of the conditions we have discussed in this article, ION shares a list of common causes that can be found with all types of retinal vascular disorders: In addition to the risk factors already mentioned, some of the other possible causes of ION are:
- Rheumatoid arthritis
- Herpes Zoster
- Anemia
- Syphilis
- Low blood pressure or severe high blood pressure
- Some cardiac diseases
- Vasculitis
- Gastro-intestinal diseases
Treatment of ION
The following has been taken from the American Academy of Ophthalmology: “At this time, there is no proven effective treatment for non-arteritic anterior ischemic optic neuropathy (NAION). Sometimes, corticosteroids may be given to help reduce the inflammation associated with the condition, but the effectiveness of this treatment option is still inconclusive.” As with each of the conditions addressed in this article, it is important to try and control the underlying cause of cardiovascular disease (a risk factor for NAION) to minimise further vision loss. For the more dangerous form – Arteritic AION – corticosteroids are given to protect the non affected eye. Ischemic Optic Neuropathy in all it’s forms makes up a complex group of conditions. We will be revisiting the topic of ION over the coming months & will address each type in more detail.
references
http://www.mdfoundation.com.au
https://www.aao.org
http://blogs.nejm.org
https://medlineplus.gov
https://www.snec.com.sg
https://www.ncbi.nlm.nih.gov