Back to Basics-Diabetic retinopathy
Retinal Disorders
Diabetic Retinopathy
Continuing with our look at common eye conditions, one that must be discussed is Diabetic Retinopathy.
What is Diabetes?
Before we investigate Diabetic Retinopathy we should first look at Diabetes itself. Diabetes is a group of conditions in which there is too much glucose in the blood. Glucose is the main source of energy for the body and comes from carbohydrate foods we eat. The body breaks carbohydrate foods down to glucose which then enters the blood stream. For glucose to enter the cells to be used for energy, a hormone called insulin must be available. Insulin is produced by cells found in the pancreas.
Diabetes occurs when the body either does not make insulin or the insulin that is produced by the pancreas is not working properly. This leads to increased blood glucose (sugar) levels which can lead to the development of diabetes.
There are two main types of Diabetes: Type 1 Diabetes and Type 2 Diabetes.
Type 1 Diabetes
Type 1 Diabetes is an autoimmune disease that occurs when the pancreas is no longer able to produce the insulin needed, because the cells that produce the insulin have been destroyed by the body’s immune system.
Usually diagnosed in childhood, teen and young adult years, type 1 diabetes can occur at any age. Lifestyle choices don’t cause type 1 diabetes.
Type 2 Diabetes
Type 2 diabetes is a chronic condition that occurs when the pancreas does not produce enough insulin and / or the insulin does not work effectively to meet the body’s needs.
It represents the majority of all cases of diabetics in Australia; 85-90% according to statistics released by Diabetes NSW™. It is more likely to develop in people with a family history of the disease and usually develops in adults over the age of 45 years. Unfortunately in recent years there has been an increased incidence in younger age groups. Unlike Type 1 Diabetes, Type 2 Diabetes can be delayed or prevented in 58% of cases.
What is Diabetic Retinopathy?
Diabetic Retinopathy affects blood vessels in the light-sensitive tissue called the retina that lines the back of the eye. It is the most common cause of vision loss among diabetics and the leading cause of vision impairment and blindness among working-age adults.
There are three main types of diabetic retinopathy:
- Non-proliferative retinopathy is an early form of the disease, where the retinal blood vessels leak fluid or bleed.
- Macular oedema is a swelling of the macula, caused by the leakage of fluid from retinal blood vessels. It can damage central vision.
- Proliferative retinopathy (PDR) is an advanced form of the disease and occurs when blood vessels in the retina disappear and are replaced by new fragile vessels that bleed easily, and that can result in a sudden loss of vision.
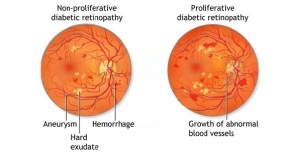
image of two retinal images showing the different types of diabetic retinopathy. Image courtesy of http://www.isotineeyedrops.com

Fundus photo of a 55yo male which shows significant diabetic changes: cotton wool spots, dot and blot haemorrhages and hard exudates
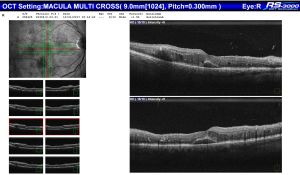
The OCT that corresponds with the above retinal photo demonstrates intra-retinal cysts and sub retinal fluid (diabetic macula oedema)
What causes Diabetic Retinopathy?
Essentially poorly controlled blood sugar levels in diabetic patients over a long period of time is what causes Diabetic retinopathy; Chronically high blood sugar is associated with damage to the tiny blood vessels in the retina, leading to diabetic retinopathy. Diabetic retinopathy can cause blood vessels in the retina to haemorrhage, which distorts vision. In its most advanced stage, new abnormal blood vessels ‘proliferate’ (increase in number) on the surface of the retina, which can lead to scarring and cell loss in the retina.
What is the treatment for Diabetic Retinopathy?
“The most important factor in the medical management of diabetic retinopathy is good glycaemic control, which is associated with reduced risk of newly diagnosed retinopathy and of progression of existing retinopathy.” [Diabetes Control and Complications Trial-United Kingdom Proliferative Diabetic Retinopathy Study (DCCT-UKPDS)].
As diabetic retinopathy becomes more severe, comprehensive dilated eye exams are needed more frequently. People with severe non-proliferative diabetic retinopathy have a high risk of developing proliferative diabetic retinopathy and may need a comprehensive dilated eye exam as often as every 2 to 4 months. Our retinal specialist Dr Daniel Polya suggests some of the things an ophthalmologist is looking for when performing a comprehensive eye examination in a diabetic patient:
- changes to the blood vessels / leaking blood vessels
- Swelling in the macula – macula oedema
- changes in the lens
If macula oedema or severe diabetic retinopathy is suspected, we may perform a fluorescein angiogram to look for damaged or leaky blood vessels. You can find more information about fluorescein angiography in our blog on Macular degeneration.
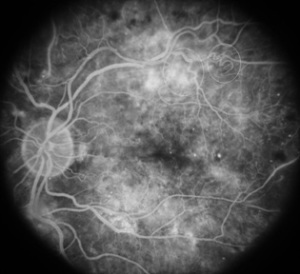
Fluorescein Angiography showing abnormal vessels and profuse leakage from damaged vessels. http://www.retinaeye.com
For proliferative diabetic retinopathy (PDR) there are several treatment options: Anti-VEGF drugs (bevacizumab, ranibizumab, aflibercept) are the most commonly used treatments. Laser and surgery are also options.
For diabetic macula oedema, laser therapy, Anti-VEGF drugs and steroid injections are all available treatment options.
To learn more about these treatment options, book your diabetic eye examination with Sydney Ophthalmic Specialists on (02) 9241 2913.
references
http://www.diabetessa.com.au
http://diabetesnsw.com.au
https://nei.nih.gov
https://www.aao.org
http://www.isotineeyedrops.com

