Back to Basics – Macular Degeneration
Retinal Disorders
Macular Degeneration
This week we are looking at the Retina & some of the conditions which affect the function of the retina. Today the focus is on Macular degeneration.
What is Macular Degeneration?
Macular Degeneration is also referred to as Age Related Macular Degeneration or AMD as it generally affects people as they age. There is a genetic component to macular degeneration and the onset can vary from person to person depending on the condition of their macula. The macula (fovea) is a small area in the centre of the retina. It is the part of the eye that we use to read and see fine detail. The macula consists of several layers of tiny cells and as we get older, some of these can fail to function properly. This can lead to a build-up of deposits in the retina and the growth of new blood vessels. Unfortunately, these new blood vessels are fragile and bleed easily. If this happens, there may be a sudden loss of central vision and objects may appear distorted. Below is an image of a healthy retina, as seen through an ophthalmoscope. 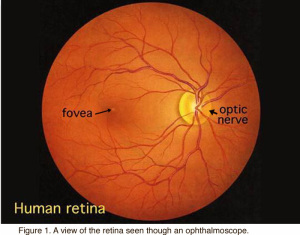 Macular Degeneration presents as one of two forms: Wet or Dry. Dry AMD is the more common of the two forms. It is an early stage of the disease related to ageing and thinning of macula tissues or depositing of cellular debris, called drusen, in the macula, creating shadowy or blurry spots in the central vision field. In its later stages, the blind spots can grow and darken. Wet AMD is a more advanced and damaging form of the disease. As the retina is starved of oxygen, new blood vessels grow behind the retina, underneath the macula in order to resupply oxygen to the retina. These new blood vessels are weak and fragile, leading to them leak blood and fluid which causes the macula to swell. Vision loss can happen rapidly with this stage if the blood vessels haemorrhage. The damage caused by the blood vessels can also scar the retina. Symptoms can include distortion in vision; straight lines may appear wavy. Blind spots can also appear in the central vision. [https://www.hollows.org.nz]
Macular Degeneration presents as one of two forms: Wet or Dry. Dry AMD is the more common of the two forms. It is an early stage of the disease related to ageing and thinning of macula tissues or depositing of cellular debris, called drusen, in the macula, creating shadowy or blurry spots in the central vision field. In its later stages, the blind spots can grow and darken. Wet AMD is a more advanced and damaging form of the disease. As the retina is starved of oxygen, new blood vessels grow behind the retina, underneath the macula in order to resupply oxygen to the retina. These new blood vessels are weak and fragile, leading to them leak blood and fluid which causes the macula to swell. Vision loss can happen rapidly with this stage if the blood vessels haemorrhage. The damage caused by the blood vessels can also scar the retina. Symptoms can include distortion in vision; straight lines may appear wavy. Blind spots can also appear in the central vision. [https://www.hollows.org.nz]
What causes Macular Degeneration?
As mentioned, there is a genetic component to AMD, however other factors that increase the risk of AMD have been identified. Our retinal specialist Dr Daniel Polya reports that “smoking, high blood pressure and a family history of the disease can increase the risk of developing macular degeneration”. Dr Polya also recommends regular eye exams to help detect macular degeneration early, which could prevent permanent vision loss.
What are the symptoms of Macular Degeneration?
As the macular is responsible for central vision, symptoms of AMD are often detected soon after the onset of the disease. Some of the possible symptoms include:
- Loss of ability to see objects clearly
- Gradual loss of colour vision
- Distorted or blurry vision
- A dark or empty area appearing in the centre of vision
How is Macular degeneration diagnosed?
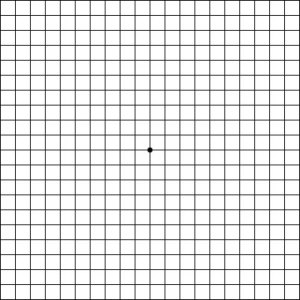
Modern technology has helped in early and prompt diagnosis of AMD. When looking for AMD, your ophthalmologist will perform a dilated retinal examination & may request some additional tests such as an OCT (Optical Coherence Tomography), Retinal Photo or a Fundus fluorescein angiography (FFA). Each of these tests are used to examine the tiny blood vessels in the retina. In an FFA procedure, a dye called Fluorescein is injected into the patient’s vein to examine the blood flow of the retina. There is also a very simple test you can perform at home called the Amsler Grid (see image below). If the grid lines are wavy, broken or distorted, or if there are blurred or missing patches, this may be a symptom of macular degeneration.
To download your own Amsler grid click on the following link http://www.mdfoundation.com.au/resources/1/amsler_grid.pdf
our OCT at Sydney Ophthalmic Specialists has been used to help detect and diagnose retinal conditions
How is Macular Degeneration treated?
The Macular Disease Foundation Australia® advise that there is currently no medical treatments available for dry macular degeneration, however a substantial amount of research is being conducted to find a treatment. A large American study, the Age-Related Eye Diseases Study (AREDS), found that certain combinations of vitamins could reduce the chance of AMD getting worse by about one quarter. This was indicated for both Dry and Wet AMD. In addition to vitamin supplements, it is advised to quit smoking & make certain dietary changes. There are several foods which promote macular health, including nuts & fish oils. For Wet AMD the most common form of treatment is with a drug referred to as anti-VEGF. A protein called Vascular Endothelial Growth Factor (VEGF) is predominantly responsible for the leaking and growth of the new blood vessels in wet macular degeneration. To slow or stop this process various drugs that block this protein (called anti-VEGFs) may be injected into the eye. Clinical trials have shown that the use of anti-VEGF drugs maintains vision in the vast majority of wet macular degeneration patients. These anti-VEGF drugs are administered as injections into the eye. The usual treatment regimen begins with monthly injections for three months. Then to maintain control of the disease injections must usually be continued on an indefinite basis. The interval between these ongoing injections is determined on an individualised basis by the eye specialist in consultation with the patient. Lucentis® (ranibizumab), Eylea® (aflibercept), Avastin® (bevacizumab) The choice of the most appropriate drug should be discussed with the eye specialist. For any inquiries regarding the treatment of Macular Degeneration, and to make an appointment with our retinal specialist Dr Dan Polya, please phone our rooms on (02) 9241 2913. References
http://www.cphospital.com.au/
http://www.mdfoundation.com.au
https://www.hollows.org.nz