Back to Basics-Retinal Detachment
Retinal Disorders
Retinal Detachment
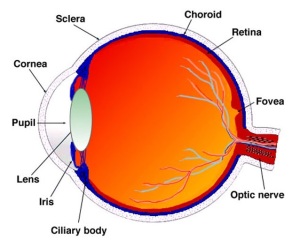
We have been looking at the retina this week as part of our back to basics series. As discussed, the retina is the light-sensitive layer of tissue that lines the inside of our eye and sends visual messages through the optic nerve to our brains.
When discussing retinal detachments, it is necessary to look at the anatomy in a little more detail. The retina is composed of ten layers but can be broken down into two main parts; the outer retinal pigment epithelium (RPE) and the inner neural retina. The RPE is a single layer of cells, while the inner neural retina is comprised of nine layers. This makes up the ten layers of the retina which we discussed earlier in the week. Our blog post where we looked at the anatomy of the retina can be found here: https://sosdoctors.com.au/back-to-basics-the-retina/
The vitreous makes up the largest volume of the eye and provides support for the delicate inner structures of the eye. The gel-like substance helps the eye maintain it’s round shape. There are millions of fine fibres intertwined within the vitreous that attach the vitreous to the retina. The attachment is strongest at the optic disc and the fovea.
The choroid is the layer behind the retina, which contains blood vessels that nourish parts of the retina.
What is a retinal detachment?
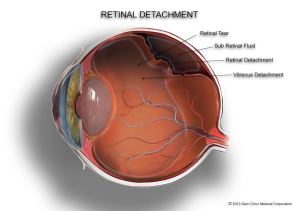
As the name suggests, a retinal detachment occurs when the retina separates from the inner lining within the eye. While not common, it is a very serious condition. Retinal detachments are often associated with holes or tears in the retina. If not treated promptly retinal detachment may lead to partial or complete loss of vision. Click on the image below to see what happens in a retinal detachment.
What causes retinal detachment?
It is important to note that while we know of many causes of retinal detachments, most detachments do not have any clear precipitating factor. As we get older, the vitreous inside our eye may change shape and pull away from the retina, this is called a posterior vitreous detachment & in itself does not pose a threat to vision. However if when the vitreous pulls away from the retina & pulls with it a piece of the retina, this is called a retinal tear and is probably the most common causes of a detached retina.
Retinal holes and tears are small breaks in the retina and do not necessarily affect vision straight away. However as holes and tears can allow fluid to escape and build up behind the retina, these holes and tears can lead to a detachment as the retina is lifted off the back wall of the eye. When the retina detaches, it separates from it’s nourishing blood supply and collapses into the posterior cavity of the eye resulting in loss of vision. There are three main types of retinal detachment:
- Rhegmatogenous – [pronounced reg-ma-tah-jenous] is a tear or break in the retina allowing fluid to escape under the retina, separating it from the RPE (outer most layer). These are the most common forms of retinal detachments.
- Tractional – caused by scar tissue on the surface of the retina contracting and separating the retina from the RPE. We see this type of detachment less commonly.
- Exudative – This form of retinal detachment is caused by retinal disease, including inflammatory disorders and injury or trauma to the eye. In this type of retinal detachment, fluid leaks under the retina, but there are no tears or breaks in the retina. Click the image below to enlarge.
Retinal detachments can occur at any age and are more commonly seen in men than women. They are likely to occur in people who have a high degree of myopia / short sightedness, have a history of detachment in the other eye or a family history of retinal detachment. Other risk factors include eye injuries / trauma to the eye, a history of cataract surgery or the presence of an inflammatory eye disease such as degenerative myopia, uveitis or lattice degeneration (retinal thinning).
What are the signs and symptoms of retinal detachment?
Retinal detachment causes sudden loss of part or all of your vision in the eye affected. It is painless & is often preceded by floaters and marked flashing lights. The floaters that can precede a detachment are often reported as looking like little “cobwebs” in the vision. A ‘curtain’ or ‘shadow’ appearing in the peripheral vision is an indication of a visual field defect & if experienced, one should urgently seek the attention of an ophthalmologist. It is important to remember that a retinal detachment is considered a medical emergency.
How is retinal detachment treated?
The treatment of a retinal detachment is determined by the type of detachment. Various treatment options are available and in some cases it is necessary to perform more than one operation. Treatment options include:
- Laser photocoagulation, which uses a laser to seal retinal tears in the early stages and is performed in our clinic.
- Scleral buckle surgery, which involves supporting the retinal breaks with a silicone band that is placed around the eye.
- Freezing or Cryopexy, which involves freezing the sclera behind the retinal tear. This is usually performed in conjunction with scleral buckle surgery.
- Vitrectomy, this is used in complex cases of detachment and involves removing the vitreous and filling the space inside the eye with gas or less frequently, oil.
Visual outcome post operatively is not always predictable & it can take months before the final visual result is known. Visual results are best if the repair is performed before the macula detaches. This is why it is important to contact an ophthalmologist immediately if you see a sudden or gradual increase in the number of floaters and or flashes of light or if a dark ‘curtain’ falls over your field of vision.
If you suspect changes to the floaters in your vision call us on (02) 9241 2913 to make an appointment for an eye examination with one of our ophthalmologists.
references
https://www.betterhealth.vic.gov.au
http://www.cphospital.com.au/
https://nei.nih.gov/health
https://www.aao.org
http://patient.info/health/retinal-detachment-leaflet